Abstract
Purpose
A body mass index (BMI) > 35 kg/m2 is a relative contraindication to heart transplantation in patients with end-stage heart failure. Bariatric surgery can be considered either concomitantly with continuous-flow left ventricular assist device (CF-LVAD) placement, or staged after CF-LVAD has been placed. We sought to evaluate the outcomes of these approaches.
Materials and Methods
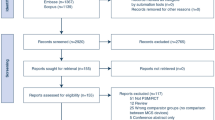
An electronic search was performed to identify all relevant studies. After assessment for inclusion and exclusion criteria, eight studies were pooled for systematic review and metaanalysis.
Results
Overall, of 59 patients, 22 (37%) underwent simultaneous sleeve gastrectomy with CF-LVAD implantation while 37 (63%) underwent staged sleeve gastrectomy after CF-LVAD. The mean age of patients was 46 years (95% CI: 39–53) with 40% females. Mean BMI at most recent follow-up (33.4 kg/m2, 95% CI: 30.2–36.6) was significantly lower compared with mean preoperative BMI (46.7 kg/m2, 95% CI: 42.9–50.6) (p < 0.01). There was no significant difference in total incidence of postoperative complications (simultaneous, 16% (95% CI: 1–87%) versus staged, 23% (95% CI: 7–53%)) or in overall survival (simultaneous, 93% (95% CI: 72–99%) versus staged, 79% (95% CI: 60–90%), p = 0.17) for average follow-up time of 12.7 months. Bariatric surgery resulted in 66% of patients (95% CI: 51–79) to be listed for heart transplantation, including 33% (95% CI: 22–47) who were transplanted.
Conclusions
Both simultaneous and staged bariatric surgeries with CF-LVAD placement have comparable outcomes and significantly reduce BMI. This can allow previously ineligible patients to undergo heart transplantation.



Similar content being viewed by others
References
Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity among adults and youth: United States, 2015-2016. NCHS Data Brief. 2017:1–8.
Kenchaiah S, Evans JC, Levy D, et al. Obesity and the risk of heart failure. N Engl J Med. 2002;347:305–13.
Sardu C, De Lucia C, Wallner M, et al. Diabetes mellitus and its cardiovascular complications: new insights into an old disease. J Diabetes Res. 2019;2019:1905194–2. https://doi.org/10.1155/2019/1905194.
Lopez-Jimenez F, Cortes-Bergoderi M. Update: systemic diseases and the cardiovascular system (i): obesity and the heart. Rev Esp Cardiol. 2011;64:140–9. https://doi.org/10.1016/j.recesp.2010.10.010.
Kindel TL, Strande JL. Bariatric surgery as a treatment for heart failure: review of the literature and potential mechanisms. Surg Obes Relat Dis. 2018;14:117–22. https://doi.org/10.1016/j.soard.2017.09.534.
Koliaki C, Liatis S, Kokkinos A. Obesity and cardiovascular disease: revisiting an old relationship. Metabolism. 2019;92:98–107. https://doi.org/10.1016/j.metabol.2018.10.011.
Bour ES. Evidence supporting the need for bariatric surgery to address the obesity epidemic in the United States. Curr Sports Med Rep. 2015;14:100–3. https://doi.org/10.1249/JSR.0000000000000135.
Greene J, Tran T, Shope T. Sleeve Gastrectomy and left ventricular assist device for heart transplant. JSLS. 2017;21:e2017.00049. https://doi.org/10.4293/JSLS.2017.00049.
Ovrebo B, Strommen M, Kulseng B, et al. Bariatric surgery versus lifestyle interventions for severe obesity: 5-year changes in body weight, risk factors and comorbidities. Clin Obes. 2017;7:183–90. https://doi.org/10.1111/cob.12190.
Mehra MR, Canter CE, Hannan MM, et al. The 2016 International Society for Heart Lung Transplantation listing criteria for heart transplantation: a 10-year update. J Heart Lung Transplant. 2016;35:1–23. https://doi.org/10.1016/j.healun.2015.10.023.
Lietz K, Miller LW. Patient selection for left-ventricular assist devices. Curr Opin Cardiol. 2009;24:246–51. https://doi.org/10.1097/HCO.0b013e32832a0743.
Winters GL, Kendall TJ, Radio SJ, et al. Posttransplant obesity and hyperlipidemia: major predictors of severity of coronary arteriopathy in failed human heart allografts. J Heart Transplant. 1990;9:364–71.
Jalowiec A, Grady KL, White-Williams C. Clinical outcomes in overweight heart transplant recipients. Heart Lung. 2016;45:298–304. https://doi.org/10.1016/j.hrtlng.2016.03.005.
Jeng EI, Aranda Jr JM, Ahmed M, et al. Left ventricular assist device and bariatric surgery: a bridge to heart transplant by weight and waiting time reduction. J Card Surg. 2016;31:120–2. https://doi.org/10.1111/jocs.12688.
Ionut V, Bergman RN. Mechanisms responsible for excess weight loss after bariatric surgery. J Diabetes Sci Technol. 2011;5:1263–82. https://doi.org/10.1177/193229681100500536.
Ulker İ, Yildiran H. The effects of bariatric surgery on gut microbiota in patients with obesity: a review of the literature. Biosci Microbiota Food Health. 2019;38:3–9. https://doi.org/10.12938/bmfh.18-018.
Garb J, Welch G, Zagarins S, et al. Bariatric surgery for the treatment of morbid obesity: a meta-analysis of weight loss outcomes for laparoscopic adjustable gastric banding and laparoscopic gastric bypass. Obes Surg. 2009;19:1447–55. https://doi.org/10.1007/s11695-009-9927-2.
Pories WJ. Bariatric surgery: risks and rewards. J Clin Endocrinol Metab. 2008;93:S89–96. https://doi.org/10.1210/jc.2008-1641.
Khan S, Rock K, Baskara A, et al. Trends in bariatric surgery from 2008 to 2012. Am J Surg. 2016;211:1041–6. https://doi.org/10.1016/j.amjsurg.2015.10.012.
Rosenthal RJ, Diaz AA, Arvidsson D, et al. International sleeve gastrectomy expert panel consensus statement: best practice guidelines based on experience of >12,000 cases. Surg Obes Relat Dis. 2012;8:8–19. https://doi.org/10.1016/j.soard.2011.10.019.
Gagner M, Buchwald JN. Comparison of laparoscopic sleeve gastrectomy leak rates in four staple-line reinforcement options: a systematic review. Surg Obes Relat Dis. 2014;10:713–23. https://doi.org/10.1016/j.soard.2014.01.016.
Gregoric ID, Radovancevic R, Patel MK, et al. Laparoscopic sleeve gastrectomy in morbidly obese patients undergoing left ventricular assist device implantation. J Heart Lung Transplant. 2018;37:S277. https://doi.org/10.1016/j.healun.2018.01.695.
Shah SK, Gregoric ID, Nathan SS, et al. Simultaneous left ventricular assist device placement and laparoscopic sleeve gastrectomy as a bridge to transplant for morbidly obese patients with severe heart failure. J Heart Lung Transplant. 2015;34:1489–91. https://doi.org/10.1016/j.healun.2015.06.011.
Hawkins RB, Go K, Raymond SL, et al. Laparoscopic sleeve gastrectomy in patients with heart failure and left ventricular assist devices as a bridge to transplant. Surg Obes Relat Dis. 2018;14:1269–73. https://doi.org/10.1016/j.soard.2018.04.005.
Punchai S, Nor Hanipah Z, Sharma G, et al. Laparoscopic sleeve gastrectomy in heart failure patients with left ventricular assist device. Obes Surg. 2019;29:1122–9. https://doi.org/10.1007/s11695-018-3570-8.
Lamba HK, Santiago A, Kurihara C, et al. Bariatric surgery in patients with continuous flow left ventricular assist devices. J Heart Lung Transplant. 2018;37:S385–6. https://doi.org/10.1016/j.healun.2018.01.992.
Zolty R, Um J, Raichlin E, et al. Abstract 16793: laparoscopic sleeve gastrectomy in morbidly obese patients with end-stage heart failure and LVAD. Circulation. 2016;134:A16793. https://doi.org/10.1161/circ.134.suppl_1.16793.
Zenilman A, Pechman D, Moran-Atkin E, et al. Bariatric surgery in patients with left ventricular assist devices: a safe and effective method of weight loss as a gateway to heart transplantation. Surg Obes Relat Dis. 2019;15:1780–4. https://doi.org/10.1016/j.soard.2019.08.003.
Poglajen G, Kumar S, Akkanti B, et al. The combination of left ventricular assist device and laparoscopic sleeve gastrectomy may promote myocardial recovery in obese advanced chronic heart failure patients. J Heart Lung Transplant. 2019;38:S81–2. https://doi.org/10.1016/j.healun.2019.01.187.
Vest AR, DeNofrio A, Coston A, et al. Impact of early weight changes after left ventricular assist device implantation on subsequent survival. J Card Fail. 2018;24:S18. https://doi.org/10.1016/j.cardfail.2018.07.053.
Vandersmissen K, Driesen J, Van den Bossche K, et al. Do LVAD patients need a specific diet to control weight? J Heart Lung Transplant. 2017;36:S176–7. https://doi.org/10.1016/j.healun.2017.01.464.
Vest AR, Patel P, Schauer PR, et al. Clinical and echocardiographic outcomes after bariatric surgery in obese patients with left ventricular systolic dysfunction. Circ Heart Fail. 2016;9:e002260. https://doi.org/10.1161/CIRCHEARTFAILURE.115.002260.
Nadalini L, Zenti MG, Masotto L, et al. Improved quality of life after bariatric surgery in morbidly obese patients. Interdisciplinary group of bariatric surgery of Verona (G.I.C.O.V.). G Chir. 2014;35:161–4.
Lim C-P, Fisher OM, Falkenback D, et al. Bariatric surgery provides a “bridge to transplant” for morbidly obese patients with advanced heart failure and may obviate the need for transplantation. Obes Surg. 2016;26:486–93. https://doi.org/10.1007/s11695-015-1789-1.
Smith ME, Ghaferi AA. Understanding the benefits of bariatric surgery: how much evidence is enough? JAMA Surg. 2018;153:e183332. https://doi.org/10.1001/jamasurg.2018.3332.
Gulliford MC, Charlton J, Prevost T, et al. Costs and outcomes of increasing access to bariatric surgery: cohort study and cost-effectiveness analysis using electronic health records. Value Health. 2017;20:85–92. https://doi.org/10.1016/j.jval.2016.08.734.
Flanagan E, Ghaderi I, Overby DW, et al. Reduced survival in bariatric surgery candidates delayed or denied by lack of insurance approval. Am Surg. 2016;82:166–70.
Craig H, le Roux C, Keogh F, et al. How ethical is our current delivery of care to patients with severe and complicated obesity? Obes Surg. 2018;28:2078–82. https://doi.org/10.1007/s11695-018-3301-1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Statement of Human and Animal Rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
For this type of study, formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Challapalli, J., Maynes, E.J., O’Malley, T.J. et al. Sleeve Gastrectomy in Patients with Continuous-Flow Left Ventricular Assist Devices: a Systematic Review and Meta-Analysis. OBES SURG 30, 4437–4445 (2020). https://doi.org/10.1007/s11695-020-04834-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04834-4